Improving Mastitis Treatments by Targeted Antimicrobial Therapy
Published: October 14, 2016
By: Pamela L. Ruegg, DVM, MPVM, University of WI, Dept. of Dairy Science, Madison WI
Introduction
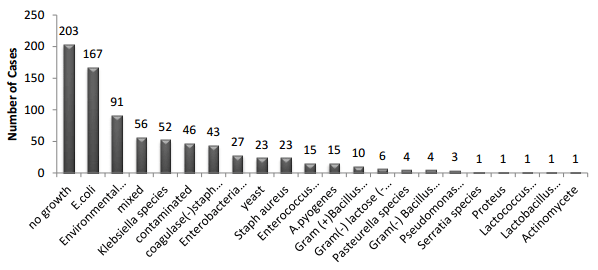
Control of mastitis caused by Streptococcus agalactiae and Staphylococcus aureus has resulted in reductions in bulk tank somatic cell count (SCC) but many herds continue to struggle with treatment of clinical mastitis caused by environmental pathogens. On many modern dairy farms, mastitis is caused by an increasingly diverse group of opportunistic pathogens (Figure 1). Common environmental mastitis pathogens include both Gram negative bacteria and Gram positive bacteria (Figure 1). The presentation of the symptoms and duration of infection is associated with the degree of host adaptation of the pathogen. Some environmental pathogens (such as most E. coli), are truly opportunistic and the immune response successfully eliminates them after a brief period of mild clinical disease. Other environmental pathogens (such as Streptococci spp.) have become more host adapted and may present as mild clinical cases that erroneously appear to resolve when the case has actually returned to a subclinical state. Both of these scenarios make it very difficult to determine success of mastitis treatments. While farmers often remember the most severe cases of mastitis, research demonstrates that the majority of clinical mastitis cases are mild to moderate in severity. The purpose of this presentation is to review research based principles that can help improve treatment of clinical mastitis.
Figure 1. Results of milk samples submitted from 793 cases of clinical mastitis occurring on 51 large Wisconsin dairy farms in 2010.1
DETERMINING RELEVANT OUTCOMES OF MASTITIS THERAPY
It is often difficult to determine if mastitis treatments are successful because there is no standard outcome that is used to evaluate outcomes. The detection of mastitis is based on recognition of the immune response that is a result of the infection. Thus, interpretation of treatment outcomes can be confusing because, clinical signs will normally resolve within 4-6 days, regardless of treatment. This is expected, as the response of immunologically competent cows will often successfully reduce the number of bacteria infecting the gland. However, disappearance of clinical signs does not always indicate that the infection has been successfully eliminated. As the immune response lessens, the milk may return to normal appearance, however many of these cases may have simply regressed to a subclinical state and maintain increased SCC. This occurrence is especially true for Gram positive pathogens.
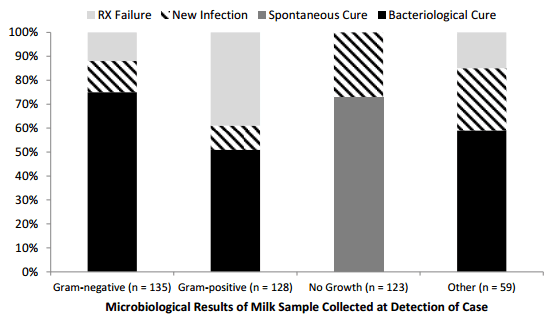
The ability to achieve a bacteriological cure depends on the pathogen, case severity, variation in immune response among cows, efficacy of the treatment protocol (when needed) and the promptness of initiating treatment.2 Even in the absence of mastitis caused by Staph aureus, bacteriological cures are almost always greater for Gram negative as compared to Gram positive pathogens (Figure 2).1
Figure 2. Treatments outcomes based on comparison of microbiological results of Milk samples collected at detection of clinical case and follow-up samples collected 3 weeks later.1
In one study, bacteriological cure was 7 times more likely for first cases of mastitis as compared to recurrent cases.3 Definition and interpretation of bacteriological cure also depends on laboratory procedures as differences in laboratory protocols can influence the probability of recovering bacteria from milk samples. Issues such as the frequency of sampling, the volume of milk that is inoculated, the time period after therapy until sampling and time between collection of consecutive samples all contribute to the wide variation in bacteriological cure rates noted in the literature.4
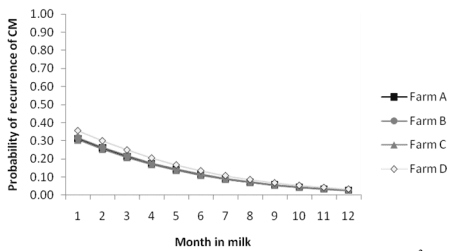
On a practical basis, farmers often assess clinical efficacy based on the appearance of the milk or other indicators such as recurrence of another clinical case, reduction in SCC, return of milk yield to normal, retention of the cow within the herd and number of days milk is discarded (because of abnormal appearance or the presence of antibiotic residues). Recurrence of another case of clinical mastitis is one of the least desirable outcomes after treatment and may be more likely for cases that occur early in lactation as compared to cases that occur later (Figure 3)3. This may indicate the need for more aggressive treatment protocols (for example, longer duration therapy) for cows experiencing mastitis in early lactation as compared to treatments for cases that occur later.
Figure 3. Recurrence of clinical mastitis (CM) by stage of lactation3
Somatic cell reduction below 200,000 cells /mL is another desired outcome but occurs slowly and this outcome is highly influenced by pathogen. Of cases caused by Gram-negative pathogens or no growth 63% resulted in somatic cell reductions to less than 200,000 cell/mL within 21-55 days after treatment in contrast to only 44% of cases caused by Gram-positive bacteria.3 While long-term reductions in SCC should occur after successful therapy, shortterm changes in SCC should not be used to determine when to stop therapy nor to determine if therapy has been effective. Likewise, the use of cowside tests like the California Mastitis Test should not be used to determine when to stop treatment.
Cow Factors Influencing Treatment Outcomes.
Host factors are well known to influence the probability of success responses to mastitis infections.5 Older cattle have a greater risk of both subclinical and clinical mastitis and several studies have indicated that older cattle have poorer responses to treatment as compared to younger cattle.6 Deluyker et al., used a rigorous definition of clinical cure (normal milk by 5 d and no relapse within 3 weeks post-treatment) and reported a reduction in combined “clinical & bacteriological cure rates” from 39% (lactation 1) to 26-30% for older cattle.7 Other researcher have reported that bacteriological cure after mastitis therapy were less for older cows.8-11 Age has also been associated with reduced clinical responses to therapy. Hektoen et al., measured responses to treatment by comparing scores for both acute and chronic symptoms obtained before treatment and at various periods post-treatment.12 While parity was not associated with differences in acute symptoms, the reduction in chronic symptoms (changes in the milk, gland or inflammatory response) were markedly greater in first lactation as compared to older cattle. The effect of parity should be considered by practitioners before initiating mastitis treatments. For example, when IMM compounds are approved for extended duration therapy, veterinarians may want to consider using use longer duration of treatment for cases occurring in older cows. Likewise, older cows (>3 lactation) may not be good candidates for withholding treatment if that option is used for managing some cases of mastitis on particular farms.
Differences Among Pathogens
It is well known that mastitis is caused by a diverse group of bacteria and the probability of cure is highly influenced by the characteristics of the pathogen. The pathogenesis, virulence and prognosis of IMI is influenced by important characteristics that vary among pathogens. Depending on specific virulence factors, organisms infect different locations in the mammary gland, have differing abilities to cause systemic symptoms, vary in the expected duration of subclinical phases of infection and differ in the expected rate of spontaneous bacteriological cure. Understanding these differences is fundamental to development of effective control programs. For example, expectations for spontaneous bacteriological cure of subclinical and clinical mastitis caused by Staph aureus are essentially zero13 while the expectation for spontaneous cure of E coli is quite high. 14 While a few cases may result in spontaneous cure, therapeutic cure rates for several mastitis pathogens (yeasts, pseudomonas, mycoplasma, prototheca etc.) are essentially zero, regardless of treatment. Even among Gram-positive pathogens, outcomes vary. The following typical differences among pathogens in bacteriological cure after treatment have been noted: Strep uberis (89%, n = 488 cases); Strep dysgalactiae (69%, n = 32 cases), Staph aureus (33%, n = 40 cases), and CNS (85%, n = 71).9 On farms that have controlled contagious mastitis, approximately 25-40% of clinical cases are microbiologically negative before treatment. Clinical and spontaneous cure rates for these “no-growth” samples are often very high with or without treatment.15, 16
Most cases of clinical mastitis caused by E coli are detected well after the immune response of the cow has been initiated and the immune response is usually successful in eliminating IMI caused by E coli. However, the duration of IMI caused by other coliforms (such as Klebsiella or Enterobacter) is much longer. After coliform bacteria infect the mammary gland, they multiply rapidly but most do not adhere to or invade the epithelial cells.5 If the cow's immune response is rapid and efficient, infection will be quickly eliminated and there will be little long-term impact on cow health or productivity. The outcome of clinical mastitis caused by coliform bacteria depends on the severity of the case, which is usually dependent on the balance between the dose (relative degree of exposure to bacteria) and the ability of the cow to response immunologically. Severe cases of mastitis occur most frequently in the periparturient period and early lactation and are primarily associated with characteristics of the cow that influence her ability to respond to the infection.5,17-19 When influx of neutrophils is delayed or phagocytosis or intracellular killing mechanisms of neutrophils impaired, bacterial multiplication continues, resulting in greater concentrations of inflammatory mediators and more severe clinical disease
In contrast, mastitis caused by environmental Streptococci typically respond well to IMM antimicrobial therapy but have a low spontaneous cure rate and high rate of recurrence when antimicrobials are not administered. 16 These differences among pathogen demonstrate that identification of pathogen considerably improves mastitis treatment protocols. With current laboratory methods, it is not feasible for all farms to achieve a microbiological diagnosis before beginning therapy but guiding treatment by use of on-farm culture systems (OFC) has been shown to be economically beneficial. 20,21 The use of OFC to direct treatment of clinical mastitis gives farmers the opportunity to make better treatment decisions and reduce costs associated with milk discard and treatment of microbiologically negative cases. A positively controlled clinical trial evaluating OFC demonstrated that there were no significant differences in either long-term or short-term outcomes for cases of mastitis that received treatment based on results of OFC as compared to cases treated immediately without regard to diagnosis.20,21 In this study, antimicrobials were not administered to cases that were culture negative or Gram negative thus the use of intramammary antimicrobials was reduced by approximately 50% as compared to cases which were treated without prior diagnosis. Most smaller herds cannot adopt OFC and an alternative is to encourage veterinary clinics to offer in-veterinary clinic culturing (IVCC). In these instances, farmers initiate treatment immediately but may modify treatment duration or drug after receiving a preliminary microbiological diagnosis within 24 hours. Development and oversight of a culture program (either OFC or IVCC) is an ideal way for veterinarians to increase involvement in mastitis control programs. The use of veterinary technicians to supervise these programs may also increase veterinary involvement and oversight of mastitis treatments. Veterinary technicians can visit farms to restock supplies, train farm personnel and provide oversight and quality control.
Duration of Therapy
In general, duration of antibiotic treatment should be kept as short as possible to minimize the economic losses associated with milk discard while maximizing the probability of achieving bacteriological cure. The appropriate duration of antibiotic treatment for clinical mastitis has not been well-defined and varies depending on the causative pathogen. There is considerable evidence that extended administration of antibiotics increases cure rates for pathogens that have the ability to invade secretory tissue (Staph aureus and some environmental Streps). For example, bacteriological cure for subclinical mastitis caused by Staph aureus treated with IMM ceftiofur were 0 % (no treatment), 7% (2 days), 17% (5 days) and 36% (8 days).13 Cure rates reported for clinical mastitis caused by β-lactamase negative Staph aureus were significantly greater when extended duration therapy was used (50%) versus administration of 3 treatments over 36 hours (38%).8 Likewise, bacteriological cure rates for experimentally induced Strep uberis infections increased from 58% (2-d treatment) to 69-80% for treatments of 5 or 8 days.22 Therefore, for mastitis caused by potentially invasive pathogens, the duration of therapy should be 5 to 8 days. Research to support use of extended duration therapy to treat pathogens that infect superficial tissues (for example coagulase negative staphylococci or most E. coli) has not been published and the use of extended duration therapy to treat these pathogens significantly increases costs without improving treatment outcomes.23 When extended therapy is considered, veterinarians should assess the ability of the herd personnel to perform aseptic infusions as extended intramammary treatment is associated with an increased risk of infection from opportunistic pathogens, and herds with poor infusion techniques are not good candidates for multiple doses of intramammary tubes.
Conclusion
Veterinarians should be involved in developing and implementing mastitis treatment protocols and should work with farm personnel and other professionals to actively monitor outcomes of treatments that farm personnel administer. Research evidence is available to help guide mastitis treatment decisions and to better select animals that will benefit from specific treatments. There is sufficient research evidence to help develop mastitis treatment protocols that vary depending on animal characteristics and the history of subclinical disease. The use of OFC or IVCC is an ideal way for veterinarians to become more involved in helping farmers make rational decisions about antimicrobial therapy used for treatment of mastitis.
Presented at Annual Meeting of the American Association Bovine Practitioners, Milwaukee, WI, Sept. 2013.
References
1. Oliveira, L., C. Hulland, and P. L. Ruegg. Characterization of clinical mastitis occurring in cows on 51 large dairy herds in Wisconsin. In review, J Dairy Science.
2. Hillerton JE, EA Berry. 2003. The management and treatment of environmental streptococcal mastitis. Veterinary Clinics of N Am. Food Animal Practice 19 157–169
3. Pínzon-Sanchéz, C., and P.L. Ruegg. 2011. Risk factors associated with short-term post-treatment outcomes of clinical mastitis. J Dairy Science 94:3397-3410.
4. Ruegg PL, DJ Reinemann. Milk Quality and Mastitis Tests. 2002. Bovine Practitioner. 36:41-54.
5. Burvenich C, van Merris V, Mehrzad J, et al. 2003. Severity of E. coli mastitis is mainly determined by cow factors. Vet Res 34:521.
6. Smith KL, DA Todhunter, PS Schoenberger. 1985. Environmental mastitis: cause, prevalence, prevention. J. Dairy Sci. 68:1531-1553.
7. Deluyker HA, ST Chester, SN van Oye. 1999. A multilocation clinical trial in lactating dairy cows affected with clinical mastitis to compare the efficacy of treatment with intramammary infusions of a lincosin/neomycin combination with an ampicillin/cloxacillin combination. J Vet Pharm Ther 22:274- 282.
8. Sol J, OC Sampimon, HW Barkema, YH Schukken. 2000. Factors associated with cure after therapy of clinical mastitis caused by Staphylococcus aureus. J Dairy Sci 83:278-284.
9. McDougall S, DG Arthur, MA Bryan, JJ Vermunt, AM Weir. 2007a. Clinical and bacteriological response to treatment of clinical mastitis with one of three intramammary antibiotics. New Zealand Vet J 55:161-170.
10. McDougall S, KE Agnew, R Cursons, XX Hou, CRW Compton. 2007b. Parenteral treatment of clinical mastitis with tylosin base or penethamate hydriodide in dairy cattle. J Dairy Sci 90:779-789.
11. Pyörälä S, L Kaartinen, H Kack, V Rainio. 1994. Efficacy of two therapy regimens for treatment of experimentally induced Escherichia coli mastitis in cows. J Dairy Sci 77:333-341.
12. Hektoen L, SA Odegaard, T Loken, S Larsen. 2004. Evaluation of stratification factors and scorescales in clinical trials of treatment of clinical mastitis in dairy cows. J Vet Med A 51:196-202.
13. Oliver S, RA Almeida, BE Gillespie, SJ Headrick, HH Dowlen, DL Johnson, KC Lamar, ST Chester, WM Moseley. 2004. Extended Ceftiofur therapy for treatment of experimentally-induced Streptococcus uberis mastitis in lactating dairy cattle. J Dairy Sci 87:3322-3329.
14. Suojala, L. 2010. Bovine Mastitis Caused by Escherichia coli – clinical, bacteriological and therapeutic aspects. PhD Dissertation. University of Helsinki, Finland.
15. Guterbock W M, AL Van Enennaam, R J Anderson, I A Gardner, JS Cullor, CA Holmberg. 1993. Efficacy of intramammary antibiotic therapy for treatment of clinical mastitis caused by environmental pathogens. J Dairy Sci 76: 3437-3444.
16. Morin DE, RD Shanks, GC McCoy. 1998. Comparison of antibiotic administration in conjunction with supportive measures versus supportive measures alone for treatment of dairy cows with clinical mastitis. J AM Vet Med Assoc 213:676-684.
17. Shuster DE, Lee EK, Kehrli MEJ. 1996. Bacterial growth, inflammatory cytokine production, and neutrophil recruitment during coliform mastitis in cows within ten days after calving, compared with cows at midlactation. Am J Vet Res 57:1569.
18. Vandeputte-van Messom G, Burvenich C, Roets E, et al. 1993. Classification of newly calved cows into moderate and severe responders to experimentally induced Escherichia coli mastitis. J Dairy Res 60:19.
19. Hirvonen J, Eklund K, Teppo AM, et al. 1999. Acute phase response in dairy cows with experimentally induced Escherichia coli mastitis. Acta Vet Scand 40:35.
20. Lago, A., S. M. Godden, R. Bey, P.L. Ruegg, and K. Leslie. 2011. The selective treatment of clinical mastitis based on on-farm culture results I: Effects on antibiotic use, milk withholding time and shortterm clinical and bacteriological outcomes. J Dairy Sci 84:4441-4456.
21. Lago, A., S. M. Godden, R. Bey, P.L. Ruegg, and K. Leslie. 2011. The selective treatment of clinical mastitis based on on-farm culture results II: Effects on lactation performance including, clinical mastitis recurrence, somatic cell count, milk production and cow survival. J Dairy Science 94:4457-44467.
22. Oliver S, RA Almeida, BE Gillespie, SJ Ivey, H Moorehead, P Lunn, HH Dowlen, DL Johnson, KC Lamar. 2003. Efficacy of extended pirlimycin therapy for treatment of experimentally induced Streptococus uberis intramammary infections in lactating dairy cattle. Vet Ther 4:299-308.
23. Pínzon-Sanchéz, C., V. E. Cabrera and P.L. Ruegg. 2011. Decision tree analysis of treatment strategies for mild and moderate cases of clinical mastitis. J Dairy Sci. 94:1873-1892.
Related topics:
Authors:
University of Wisconsin - USA
Recommend
Comment
Share
19 de octubre de 2016
Clinical Mastitis is easily occurs, therefore, it needs expert veterinarian which can identify the causes of this affection . If these requirements are present, all clinical mastitis cases can be treated with 100 % efficacy within 24 - 36 hours for all forms of acute mastitis and 7 - 9 days for peracute forms. Treatment of Clinical Mastitis requires knowledge of many veterinary branches. A veterinarian can becomes a pioneer in all aspects of clinical mastitis if he know the following :
- Causes of clinical mastitis under field conditions (42 causes)
- The pharmacological lines of treatment of clinical mastitis
- Good knowledge of veterinary sciences .
Recommend
Reply
19 de octubre de 2016
Best way to treat mastitis with immunomodulatory feed supplements without antimicrobials successfully treated with best results
Recommend
Reply
19 de octubre de 2016
worth reading paper regarding therapy to control biggest threat to livestock sector
Recommend
Reply
18 de octubre de 2016
Antimicrobial therapy is necessary and required in the majority of udder affections, but this category of drugs are not sufficient alone. Many other drugs and procedures are required to obtain effective and rapid therapy. There are 42 causes of clinical mastitis. The cause must be identified by expert veterinarian, but isolation then identification of the causative micro-organism delay antimicrobial therapy.
Recommend
Reply

17 de octubre de 2016
This is an excellent paper. We at Agranco, Corp. USA,
Have developed MAST-EX, oral treatment of Mastitis,
via feed, that successfully addresses the premise of this
Paper.
José E Ferrer,PhD
President
Agranco Corp. USA
WWW.AGRANCO.USA
Recommend
Reply

Would you like to discuss another topic? Create a new post to engage with experts in the community.









.jpg&w=3840&q=75)