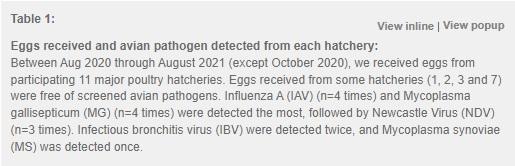
Screening Avian Pathogens in Eggs from Commercial Hatcheries in Nepal- an Effective Poultry Disease Surveillance Tool
Author details:
1.↵Yildiz D. Global Poultry Industry and Trends. 2021 Mar 11 [cited 12 Jul 2022]. In: Feed and Additive Magazine [Internet]. Available from: https://www.feedandadditive.com/global-poultry-industry-and-trends/#:~:text=The%20poultry%20sector%2C%20which%20has%20a%20market%20value%20of%20%24%20310.7,with%20a%20CAGR%20of%207%25.Google Scholar
2.↵Mottet A, Tempio G. Global poultry production: current state and future outlook and challenges. World’s Poultry Science Journal 2017; 73(2):1–12.Google Scholar
3.↵Hafez HM, Attia YA. Challenges to the Poultry Industry: Current Perspectives and Strategic Future After the COVID-19 Outbreak. Front Vet Sci. 2020 Aug 26;7:516.Google Scholar
4.↵Elhadidy M. Poultry hatcheries as potential reservoirs for antimicrobial-resistant Escherichia coli : A risk to public health and food safety. Scientific Reports 2018; 8(1)Google Scholar
5.↵Wales A, Davies R. Review of hatchery transmission of bacteria with focus on Salmonella, chick pathogens and antimicrobial resistance. World’s Poultry Science Journal 2020; 76 (3).Google Scholar
6.↵Strengthening Critical Segments of the Poultry Supply Chain. International Finance Corporation. [Cited 2022 July 12]. Available from: https://www.ifc.org/wps/wcm/connect/b226e65c-79a9-42b2-b666-2327437c3edb/NepalPoultry.pdf?MOD=AJPERES&CVID=kqMoqDKGoogle Scholar
7.↵Nepal commercial poultry survey 2071/72. Central Bureau of Statistics 2016. Available from: https://cbs.gov.np/nepalcommercial-poultry-survey-2071-072/Google Scholar
8.↵Yoo DS, Chun BC, Kim Y, Lee KN, Moon OK. Dynamics of inter-farm transmission of highly pathogenic avian influenza H5N6 integrating vehicle movements and phylogenetic information. Sci Rep. 2021;11(1):24163.Google Scholar
9.↵Parvin R, Nooruzzaman M, Kabiraj CK, Begum JA, Chowdhury EH, Islam MR, Harder T. Controlling Avian Influenza Virus in Bangladesh: Challenges and Recommendations. Viruses. 2020 Jul 12;12(7):751.Google Scholar
10.↵Board, RG, Fuller R.Humphrey TJ. Contamination of eggs with potential human pathogens. In: Board, RG, Fuller R. Microbiology of the Avian Egg 2004. Springer, Boston, MA.Google Scholar
11.↵Gantois I, Ducatelle R, Pasmans F, Haesebrouck F, Gast R, Humphrey TJ, Immerseel FV, Mechanisms of egg contamination by Salmonella Enteritidis. FEMS Microbiology Reviews 2009; 33(4): 718–738.CrossRefPubMedWeb of ScienceGoogle Scholar
12.↵Pande VV, Devon RL, Sharma P, McWhorter AR, Chousalkar KK. Study of Salmonella Typhimurium Infection in Laying Hens. Front Microbiol. 2016 Feb 25;7:203.PubMedGoogle Scholar
13.↵De Reu K, Rodenburg TB, Grijspeerdt K, Messens W, Heyndrickx M, Tuyttens FA, Sonck B, Zoons J, & Herman L. Bacteriological contamination, dirt, and cracks of eggshells in furnished cages and noncage systems for laying hens: an international on-farm comparison. Poultry science 2009; 88(11), 2442–2448.CrossRefPubMedGoogle Scholar
14.↵Roberts JR, Souillard R, Bertin J. Avian diseases which affect egg production and quality, Food Science, Technology and Nutrition 2005; 376–393.Google Scholar
15.↵Messens W, Grijspeerdt K, Herman L. Eggshell penetration by Salmonella: a review, World’s Poultry Science Journal 2005, 61:1, 71–86Google Scholar
16.↵Windhorst HW A projection of egg production until 2030. 2022 Mar 8 [cited 12 Jul 2022]. In: Zootenica International [Internet]. Available from: https://zootecnicainternational.com/focus-on/a-projection-of-egg-production-until-2030/Google Scholar
17.↵Walker S, Baum JI. Eggs as an affordable source of nutrients for adults and children living in food-insecure environments. Nutr Rev. 2022; 80(2):178–186.Google Scholar
18.↵Statistical Yearbook. Food and Agriculture Organization 2020. Available from: https://www.fao.org/3/cb1329en/CB1329EN.pdfGoogle Scholar
19.↵Zhuang QY, Wang SC, Li JP, Liu D, Liu S, Jiang WM, Chen, JM. A clinical survey of common avian infectious diseases in China. Avian diseases 2014; 58(2), 297–302.Google Scholar
20.↵Biggs PM (1982). The world of poultry disease. Avian pathology : Journal of the WVPA; 11(2), 281–300.Google Scholar
21.↵Klinkenberg D, Thomas E, Artavia FF, Bouma A. Salmonella enteritidis surveillance by egg immunology: impact of the sampling scheme on the release of contaminated table eggs. Risk Anal. 2011;31(8):1260–1270.PubMedGoogle Scholar
22.↵Crespo PS, Hernandez G, Echeita A, Torres T et al. Surveillance of foodborne disease outbreaks associated with consumption of eggs and egg products: Spain, 2002 – 2003. Eurosurveillance 2005. Available from: https://www.eurosurveillance.org/content/10.2807/esw.10.24.02726-enGoogle Scholar
23.↵Using indicator-and event-based surveillance to detect foodborne events. World Health Organization 2017. Available from: https://www.who.int/docs/default-source/documents/publications/using-indicator-and-event-base-surveillance-to-detect-foodborne-events-9789241513241-eng.pdf?sfvrsn=8e8fe021_2Google Scholar
24.↵Whiley H, Ross K. Salmonella and eggs: from production to plate. Int J Environ Res Public Health. 2015 Feb 26;12(3):2543–56.CrossRefPubMedGoogle Scholar
25.Ayala AJ, Yabsley MJ & Hernandez SM. A Review of Pathogen Transmission at the Backyard Chicken-Wild Bird Interface. Frontiers in veterinary science 2020, 7, 539925.Google Scholar
26.↵Lee M, Seo DJ, Jeon SB, Ok HE, Jung H, Choi C, Chun HS. Detection of Foodborne Pathogens and Mycotoxins in Eggs and Chicken Feeds from Farms to Retail Markets. Korean J Food Sci Anim Resour. 2016;36(4):463–8.Google Scholar
27.↵Parveen A, Rahman MM, Fakhruzzaman M et al.,. Asian J. Med. Biol. Res. June 2017, 3(2): 168–174Google Scholar
28.↵Lin Q, Chousalkar KK, McWhorter AR, Khan S. Salmonella Hessarek: An emerging food borne pathogen and its role in egg safety. Food Control 2021; 125.Google Scholar
29.↵Ter Veen C, de Wit JJ, Feberwee A. Relative contribution of vertical, within-farm and between-farm transmission of Mycoplasma synoviae in layer pullet flocks. Avian Pathol. 2020;49(1):56–61.Google Scholar
30.↵Kursa, O., Pakuła, A., Tomczyk, G. et al. Eggshell apex abnormalities caused by two different Mycoplasma synoviae genotypes and evaluation of eggshell anomalies by full-field optical coherence tomography. BMC Vet Res 15, 1 (2019). https://doi.org/10.1186/s12917-018-1758-8CrossRefGoogle Scholar
31.↵Norouzian, H., Farjanikish, G., & Hosseini, H. (2019). Molecular characterisation of Mycoplasma gallisepticum isolates from Iran in the period 2012-2017. Acta veterinaria Hungarica, 67(3), 347–359. https://doi.org/10.1556/004.2019.036Google Scholar
32.↵Landman WJ. Is Mycoplasma synoviae outrunning Mycoplasma gallisepticum? A viewpoint from the Netherlands. Avian pathology : journal of the W.V.P.A 2014; 43(1), 2–8.Google Scholar
33.↵Yadav, J. P., Tomar, P., Singh, Y., & Khurana, S. K. (2021). Insights on Mycoplasma gallisepticum and Mycoplasma synoviae infection in poultry: a systematic review. Animal biotechnology, 1–10. Advance online publication. https://doi.org/10.1080/10495398.2021.1908316Google Scholar
34.↵Galluzzo P., Migliore, S., Galuppo, L., Condorelli, L., Hussein, H. A., Licitra, F., Coltraro, M., Sallemi, S., Antoci, F., Cascone, G., Puleio, R., & Loria, G. R. (2022). First Molecular Survey to Detect Mycoplasma gallisepticum and Mycoplasma synoviae in Poultry Farms in a Strategic Production District of Sicily (South-Italy). Animals : an open access journal from MDPI, 12(8), 962.Google Scholar
35.↵Nascimento ER, Pereira VLA, Barreto ML. Avian mycoplasmosis update. Brazilian Journal of Poultry Science 2005; 7(1).Google Scholar
36.↵Feberwee JJ, Landman WJM. Induction of eggshell apex abnormalities by Mycoplasma synoviae: field and experimental studies, Avian Pathology 2009; 38:1, 77–85Google Scholar
37.Kammon A, Mulatti P, Lorenzetto M, Ferre N, Sharif M, Eldaghayes I, Dayhum A. Biosecurity and geospatial analysis of mycoplasma infections in poultry farms at Al-Jabal Al-Gharbi region of Libya. Open veterinary journal 2017, 7(2), 81–85.Google Scholar
38.↵Rabalski L, Smietanka K, Minta Z, Szewczyk B. Detection of Newcastle disease virus minor genetic variants by modified single-stranded conformational polymorphism analysis. BioMed research international 2014, 632347.Google Scholar
39.↵Lamb R, Parks G. Paramyxoviridae: the viruses and their replication. Fields Virology. 5th ed. Lippincott Williams & Wilkins 2007; Philadelphia, 1449–1496Google Scholar
40.↵Ul-Rahman A, Ishaq HM, Raza MA, Shabbir MZ. Zoonotic potential of Newcastle disease virus: Old and novel perspectives related to public health. Reviews in medical Virology 2022; 32(1)Google Scholar
41.↵Alexander DJ, Aldous EW, Fuller CM. The long view: a selective review of 40 years of Newcastle disease research, Avian Pathology 2012, 41:4, 329–335CrossRefPubMedGoogle Scholar
42.↵Silva SM, Susta L, Moresco K, Swayne DE. Vaccination of chickens decreased Newcastle disease virus contamination in eggs. Avian pathology: journal of the W.V.P.A 2006; 45(1), 38–45Google Scholar
43.↵Franzo G, Legnardi M, Tucciarone CM et al. Evolution of infectious bronchitis virus in the field after homologous vaccination introduction. Vet Res. 2019; 50, 92.Google Scholar
44.↵Wakenell P. Management and medicine of backyard poultry. Current therapy in avian medicine and surgery 2016, 550–565Google Scholar
45.↵Promkuntod N. Dynamics of avian coronavirus circulation in commercial and non-commercial birds in Asia--a review. The veterinary quarterly 2016; 36(1), 30–44.Google Scholar
46.↵Orakpoghenora O, Oladele SB, Abdu PA. Infectious Bursal Disease: Transmission, Pathogenesis, Pathology and Control - An Overview. World’s Poultry Science Journal 2020; 76(2)Google Scholar
47.↵Delmas B, Attoui H, Ghosh S, et al. ICTV virus taxonomy profile: Birnaviridae. J Gen Virol. 2019;100(1):5–6. doi:10.1099/jgv.0.001185CrossRefGoogle Scholar
48.↵Dey S, Pathak DC, Ramamurthy N, Maity HK, Chellappa MM. Infectious bursal disease virus in chickens: prevalence, impact, and management strategies. Vet Med (Auckl). 2019 Aug 5;10:85–97. doi: 10.2147/VMRR.S185159. PMID: 31497527; PMCID: PMC6689097CrossRefPubMedGoogle Scholar
49.↵Mohamed MA, Elzanaty KE, Bakhit BM, Safwat MM. Genetic characterization of infectious bursal disease viruses associated with gumboro outbreaks in commercial broilers from asyut province, egypt. ISRN Vet Sci. 2014 Feb 9;2014:916412. doi: 10.1155/2014/916412. PMID: 24977049; PMCID: PMC4060563.CrossRefPubMedGoogle Scholar
50.↵Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). Available from: https://www.cdc.gov/flu/avianflu/avian-in-birds.htmGoogle Scholar
51.↵Nomaguchi M and Adachi A (2017) Editorial: Highly Mutable Animal RNA Viruses: Adaptation and Evolution. Front. Microbiol. 8:1785. doi: 10.3389/fmicb.2017.01785CrossRefGoogle Scholar
52.↵Kosik I, Yewdell JW. Influenza Hemagglutinin and Neuraminidase: Yin−Yang Proteins Coevolving to Thwart Immunity. Viruses. 2019 Apr 16;11(4):346. doi: 10.3390/v11040346. PMID: 31014029; PMCID: PMC6520700.CrossRefPubMedGoogle Scholar
53.↵Shi W, Lei F, Zhu C, Sievers F, Higgins DG. A complete analysis of HA and NA genes of influenza A viruses. PLoS One. 2010 Dec 29;5(12):e14454. doi: 10.1371/journal.pone.0014454. PMID: 21209922; PMCID: PMC3012125.CrossRefPubMedGoogle Scholar
54.↵Capua I, Alexander DJ. Avian influenza infections in birds--a moving target. Influenza Other Respir Viruses. 2007 Jan;1(1):11–8. doi: 10.1111/j.1750-2659.2006.00004.x. PMID: 19459279; PMCID: PMC4634665.CrossRefPubMedGoogle Scholar
55.↵Bergervoet SA, Pritz-Verschuren SBE, Gonzales JL, Bossers A, Poen MJ, Dutta J, Khan Z, Kriti D, van Bakel H, Bouwstra R, Fouchier RAM, Beerens N. Circulation of low pathogenic avian influenza (LPAI) viruses in wild birds and poultry in the Netherlands, 2006-2016. Sci Rep. 2019 Sep 23;9(1):13681. doi: 10.1038/s41598-019-50170-8. PMID: 31548582; PMCID: PMC6757041.CrossRefPubMedGoogle Scholar
56.↵Shriner SA, Root JJ. A Review of Avian Influenza A Virus Associations in Synanthropic Birds. Viruses. 2020 Oct 23;12(11):1209. doi: 10.3390/v12111209. PMID: 33114239; PMCID: PMC7690888.CrossRefPubMedGoogle Scholar
57.↵Saba Shirvan A, Mardani K. Mol ecular detection of infectious bronchitis and Newcastle disease viruses in broiler chickens with respiratory signs using Duplex RT-PCR. Vet Res Forum. 2014 Fall;5(4):319–23. PMID: 25610585; PMCID: PMC4299999.PubMedGoogle Scholar
58.↵Kataria RS, Tiwari AK, Butchaiah G, Rai A. Sequence Analysis of VP2 Gene Hyper Variable Region of a Cell-culture Adapted Indian Classical Infectious Bursal Disease Virus of Chicken. Journal of Applied Animal Research 2007; 32:1, pages 49–54.Google Scholar
59.↵Kahya S, Ardicli O, Eyigor A et. al Detection of Mycoplasma gallisepticum and Mycoplasma synoviae by Real-Time PCRs and Mycoplasma gallisepticum-antibody Detection by an ELISA in Chicken Breeder Flocks. Kafkas Üniversitesi Veteriner Fakültesi Dergisi 2015; 21(3):361–366Google Scholar
60.↵Pant GR, & Selleck PW. Surveillance for Avian Influenza in Nepal 2004-2005 (Vigilancia epidemiológica para influenza aviar en Nepal durante los años 2004 y 2005). Avian Diseases. 2007; 51(1), 352–354. http://www.jstor.org/stable/4493224PubMedGoogle Scholar
61.↵National Contingency Plan for Prevention and Control of Avian Influenza in Nepal. In: World Organization for Animal Health [Internet]. Available from: https://www.woah.org/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/AvianInfluenza-Nepal.pdfGoogle Scholar
62.↵Moosavy MH, Esmaeili S, Bagheri Amiri F, Mostafavi E, Zahraei Salehi T. Detection of Salmonella spp in commercial eggs in Iran. Iran J Microbiol. 2015 Feb;7(1):50–4. PMID: 26644874; PMCID: PMC4670468.PubMedGoogle Scholar
63.↵Humphrey TJ. Contamination of egg shell and contents with Salmonella enteritidis: a review. Int J Food Microbiol. 1994;21(1-2):31–40. doi:10.1016/0168-1605(94)90197-xCrossRefPubMedWeb of ScienceGoogle Scholar
64.↵Chousalkar KK, Flynn P, Sutherland M, Roberts JR, Cheetham BF. Recovery of Salmonella and Escherichia coli from commercial egg shells and effect of translucency on bacterial penetration in eggs. Int J Food Microbiol. 2010;142(1-2):207–213. doi:10.1016/j.ijfoodmicro.2010.06.029CrossRefPubMedWeb of ScienceGoogle Scholar
65.↵Sahin O, Kobalka P, Zhang Q. Detection and survival of Campylobacter in chicken eggs. J Appl Microbiol. 2003;95(5):1070–1079. doi:10.1046/j.1365-2672.2003.02083.xCrossRefPubMedWeb of ScienceGoogle Scholar
66.↵Soler P, Hernández Pezzi G, Echeíta A, Torres A, Ordóñez Banegas Pilar, Aladueña A. Surveillance of foodborne disease outbreaks associated with consumption of eggs and egg products: Spain, 2002 - 2003. Euro Surveill. 2005;10(24):pii=2726. https://doi.org/10.2807/esw.10.24.02726-enGoogle Scholar
67.↵Egg-shell surveillance. In: USDA [Internet]. Available from: https://www.ams.usda.gov/rules-regulations/eggs#:~:text=The%20Egg%20Products%20Inspection%20Act,of%20consumers%20of%20these%20products.Google Scholar
- 1.↵
- 2.↵
- 3.↵
- 4.↵
- 5.↵
- 6.↵
- 7.↵
- 8.↵
- 9.↵
- 10.↵
- 11.↵
- 12.↵
- 13.↵
- 14.↵
- 15.↵
- 16.↵
- 17.↵
- 18.↵
- 19.↵
- 20.↵
- 21.↵
- 22.↵
- 23.↵
- 24.↵
- 25.
- 26.↵
- 27.↵
- 28.↵
- 29.↵
- 30.↵
- 31.↵
- 32.↵
- 33.↵
- 34.↵
- 35.↵
- 36.↵
- 37.
- 38.↵
- 39.↵
- 40.↵
- 41.↵
- 42.↵
- 43.↵
- 44.↵
- 45.↵
- 46.↵
- 47.↵
- 48.↵
- 49.↵
- 50.↵
- 51.↵
- 52.↵
- 53.↵
- 54.↵
- 55.↵
- 56.↵
- 57.↵
- 58.↵
- 59.↵
- 60.↵
- 61.↵
- 62.↵
- 63.↵
- 64.↵
- 65.↵
- 66.↵
- 67.↵










.jpg&w=3840&q=75)