Reserpine improves Enterobacteriaceae resistance in chicken intestine via neuro-immunometabolic signaling and MEK1/2 activation
Author details:
1. Batz, M. B., Hoffmann, S. & Morris, J. G. Ranking the disease burden of 14 pathogens in food sources in the United States using attribution data from outbreak investigations and expert elicitation. J. Food Prot. 75, 1278–1291 (2012).
2. Antunes, P., Mourao, J., Campos, J. & Peixe, L. Salmonellosis: the role of poultry meat. Clin. Microbiol. Infect. 22, 110–121 (2016).
3. Center for Disease Control and Prevention. Antibiotic Resistance Threats
Report. https://www.hhs.gov/sites/default/files/michael-craig-cdc-talkthursday-am-508.pdf (2019).
4. Fricke, W. F. et al. Antimicrobial resistance-conferring plasmids with similarity to virulence plasmids from avian pathogenic Escherichia coli strains in Salmonella enterica Serovar Kentucky isolates from poultry. Appl. Environ.
Microbiol. 75, 5963–5971 (2009).
5. Redweik, G. A. J. R., Stromberg, Z. R., Van Goor, A. & Mellata, M. Protection against avian pathogenic Escherichia coli and Salmonella Kentucky exhibited in chickens given both probiotics and live Salmonella vaccine. Poult. Sci. 99,
752–762 (2002).
6. McWhorter, A. R. & Chousalkar, K. K. A long-term efficacy trial of a live, attenuated Salmonella Typhimurium vaccine in layer hens. Front. Microbiol. 9,
1380 (2018).
7. Redweik, G. A. J. R., Jochum, J. & Mellata, M. Live bacterial prophylactics in modern poultry. Front. Vet. Sci. 7, 592312 (2020).
8. Kogut, M. H. & Arsenault, R. J. Immunometabolic phenotype alterations associated with the induction of disease tolerance and persistent asymptomatic infection of Salmonella in the chicken intestine. Front. Immunol. 8, 372 (2017).
9. Shanmugasundaram, R. et al. Effect of Salmonella infection on cecal tonsil regulatory T cell properties in chickens. Poult. Sci. 94, 1828–1835 (2015).
10. Nutma, E., Willison, H., Martino, G. & Amor, S. Neuroimmunology—the past, present, and future. Clin. Exp. Immunol. 197, 278–293 (2019).
11. Brinkman, D. J., Ten Hove, A. S., Vervoordeldonk, M. J., Luyer, M. D. & de
Jonge, W. J. Neuroimmune interactions in the gut and their significance for intestinal immunity. Cells 8, 670 (2019).
12. Cosentino, M. et al. Human CD4+CD25+ regulatory T cells selectively express tyrosine hydroxylase and contain endogenous catecholamines subserving an autocrine/paracrine inhibitory functional loop. Blood 109,
632–642 (2007).
13. Udden, S. M., Waliullah, S., Harris, M. & Zaki, H. The ex vivo colon organ culture and its use in antimicrobial host defense studies. J. Vis. Exp. 120,
55347 (2017).
14. Hassan, J. O. & Curtiss, R. Virulent Salmonella typhimurium-induced lymphocyte depletion and immunosuppression in chickens. Infect. Immun.
62, 2027–2036 (1994).
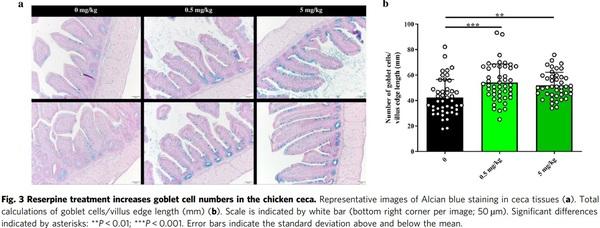
15. Forstner, J., Roomi, N., Khorasani, R., Kuhns, W. & Forstner, G. Effect of reserpine on the histochemical and biochemical properties of rat intestinal mucus. Exp. Mol. Pathol. 54, 129–143 (1991).
16. Park, C., Reid, P. E., Owen, D. A., Sanker, J. M. & Applegarth, D. A.
Morphological and histochemical changes in intestinal mucus in the reserpine-treated rat model of cystic fibrosis. Exp. Mol. Pathol. 47, 1–12 (1987).
17. Kim, Y. S. & Ho, S. B. Intestinal goblet cells and mucins in health and disease: recent insights and progress. Curr. Gastroenterol. Rep. 12, 319–330 (2010).
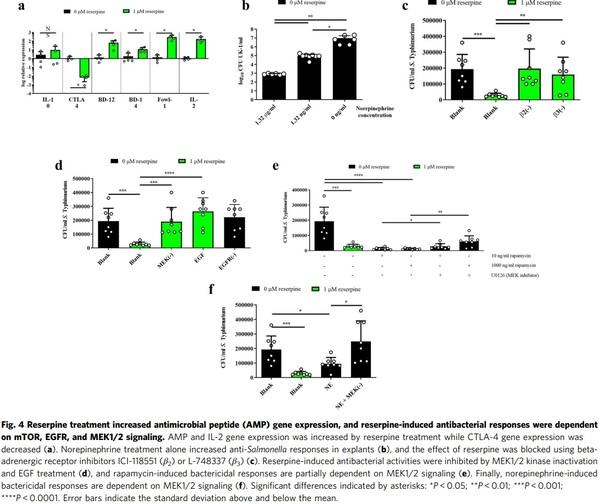
18. Couper, K. N., Blount, D. G. & Riley, E. M. IL-10: the master regulator of immunity to infection. J. Immunol. 180, 5771–5777 (2008).
19. Wing, K. et al. CTLA-4 control over Foxp3+ regulatory T cell function.
Science 322, 271–275 (2008).
20. Liao, W., Lin, J. X. & Leonard, W. J. Interleukin-2 at the crossroads of effector responses, tolerance, and immunotherapy. Immunity 38, 13–25 (2013).
21. Pol, J. G., Caudana, P., Paillet, J., Piaggio, E. & Kroemer, G. Effects of interleukin-2 in immunostimulation and immunosuppression. J. Exp. Med.
217, e20191247 (2020).
22. Arsenault, R. J., Trost, B. & Kogut, M. H. A comparison of the chicken and turkey proteomes and phosphoproteomes in the development of poultryspecific immuno-metabolism kinome peptide arrays. Front. Vet. Sci. 1, 22 (2014).
23. Zheng, C. F. & Guan, K. L. Cloning and characterization of two distinct human extracellular signal-regulated kinase activator kinases, MEK1 and
MEK2. J. Biol. Chem. 268, 11435–11439 (1993).
24. Procaccia, S., Ordan, M., Cohen, I., Bendetz-Nezer, S. & Seger, R. Direct binding of MEK1 and MEK2 to AKT induces Foxo1 phosphorylation, cellular migration, and metastasis. Sci. Rep. 7, 43078 (2017).
25. Rudd, C. E., Taylor, A. & Schneider, H. CD28 and CTLA-4 coreceptor expression and signal transduction. Immunol. Rev. 229, 12–26 (2009).
26. Meade, K. G. & O’Farrelly, C. β-Defensins: farming the microbiome for homeostasis and health. Front. Immunol. 9, 3072 (2018).
27. Sechet, E., Telford, E., Bonamy, C., Sansonetti, P. J. & Sperandio, B. Natural molecules induce and synergize to boost expression of the human antimicrobial peptide β-defensin-3. Proc. Natl Acad. Sci. USA 115, 9869–9878 (2018).
28. Xiao, Y. et al. Identification and functional characterization of three chicken cathelicidins with potent antimicrobial activity. J. Biol. Chem. 281, 2858–2867 (2006).
29. Kogut, M. H., He, H. & Kaiser, P. Lipopolysaccharide binding protein/CD14/
TLR4-dependent recognition of Salmonella LPS induces the functional activation of chicken heterophils and up-regulation of pro-inflammatory cytokine and chemokine gene expression in these cells. Anim. Biotechnol. 16,
165–181 (2005).
30. Xie, K. et al. β-Defensin 129 attenuates bacterial endotoxin-induced inflammation and intestinal epithelial cell apoptosis. Front. Immunol. 10, 2333 (2019).
31. Hop, H. et al. The key role of c-FOS for immune regulation and bacterial dissemination in Brucella infected macrophage. Front. Cell. Infect. Microbiol.
8, 287 (2018).
32. Ray, N. et al. C-Fos suppresses systemic inflammatory response to endotoxin.
Int. Immunol. 18, 671–677 (2006).
33. Okada, S., Obata, S., Hatano, M. & Tokuhisa, T. Dominant negative effect of the c-fos family gene products on inducible NO synthase expression in macrophages. Int. Immunol. 15, 1275–1282 (2003).
34. Maruyama, K. et al. c-Fos-deficient mice are susceptible to Salmonella enterica serovar Typhimurium infection. Infect. Immun. 75, 1520–1523 (2007).
35. Appleman, L. J., Berezovskaya, A., Grass, I. & Boussiotis, V. A. CD28 costimulation mediates T cell expansion via IL-2-independent and IL-2- dependent regulation of cell cycle progression. J. Immunol. 164, 144–151 (2000).
36. Krummel, M. F. & Allison, J. P. CTLA-4 engagement inhibits IL-2 accumulation and cell cycle progression upon activation of resting T cells. J.
Exp. Med. 183, 2533–2540 (1996).
37. Walker, L. S. Treg and CTLA-4: two intertwining pathways to immune tolerance. J. Autoimmun. 45, 49–57 (2013).
38. Dienz, O. et al. Accumulation of NFAT mediates IL-2 expression in memory, but not naïve, CD4+ T cells. Proc. Natl Acad. Sci. USA 104, 7175–7180 (2007).
39. Wall, R. et al. Role of gut microbiota in early infant development. Clin. Med.
Pediatr. 3, 45–54 (2009).
40. Bauer, E., Williams, B. A., Smidt, H., Verstegen, M. W. A. & Mosenthin, R.
Influence of the gastrointestinal microbiota on development of the immune system in young animals. Curr. Issues Intest. Microbiol. 7, 35–51 (2006).
41. Videnska, P. et al. Chicken faecal microbiota and disturbances induced by single or repeated therapy with tetracycline and streptomycin. BMC Vet. Res.
9, 30 (2013).
42. Lynn, M. A. et al. Early-life antibiotic-driven dysbiosis leads to dysregulated vaccine immune responses in mice. Cell Host Microbe 23, 653–660 (2018).
43. Gasparrini, A. J. et al. Persistent metagenomic signatures of early-life hospitalization and antibiotic treatment in the infant gut microbiota and resistome. Nat. Microbiol. 4, 2285–2297 (2019).
44. Crhanova, M. et al. Immune response of chicken gut to natural colonization by gut microflora and to Salmonella enterica serovar enteritidis infection.
Infect. Immun. 79, 2755–2763 (2011).
45. Bar-Shira, E., Sklan, D. & Friedman, A. Establishment of immune competence in the avian GALT during the immediate post-hatch period. Dev. Comp.
Immunol. 27, 147–157 (2003).
46. Lillehoj, H. S. & Chung, K. S. Postnatal development of T-lymphocyte subpopulations in the intestinal intraepithelium and lamina propria in chickens. Vet. Immunol. Immunopathol. 31, 347–360 (1992).
47. Van Immerseel, F. Dynamics of immune cell infiltration in the caecal lamina propria of chickens after neonatal infection with a Salmonella enteritidis strain. Dev. Comp. Immunol. 26, 355–364 (2002).
48. Dhawan, S. et al. Acetylcholine-producing T cells in the intestine regulate antimicrobial peptide expression and microbial diversity. Am. J. Physiol.
Gastrointest. Liver Physiol. 311, G920–G933 (2016).
49. Kasprowicz, D. J. et al. Stimulation of the B cell receptor, CD86 (B7-2), and the beta 2-adrenergic receptor intrinsically modulates the level of IgG1 and
IgE produced per B cell. J. Immunol. 165, 680–690 (2000).
50. Kohm, A. P. & Sanders, V. M. Norepinephrine and beta 2-adrenergic receptor stimulation regulate CD4+ T and B lymphocyte function in vitro and in vivo.
Pharmacol. Rev. 53, 487–525 (2001).
51. Gabanyi, I. et al. Neuro-immune interactions drive tissue programming in intestinal macrophages. Cell 164, 378–391 (2016).
52. Knoop, K. A. et al. Maternal activation of the EGFR prevents translocation of gut-residing pathogenic Escherichia coli in a model of late-onset neonatal sepsis. Proc. Natl Acad. Sci. USA 117, 7941–7949 (2020).
53. Bonamy, C. et al. Expression of the human antimicrobial peptide β-defensin-1 is repressed by the EGFR-ERK-MYC axis in colonic epithelial cells. Sci. Rep. 8,
18043 (2018).
54. Saxton, R. & Sabatini, D. mTOR signaling in growth, metabolism, and disease.
Cell 168, 960–976 (2017).
55. Chiang, G. G. & Abraham, R. T. Phosphorylation of mammalian target of rapamycin (mTOR) at Ser-2448 is mediated by p70S6 kinase. J. Biol. Chem.
280, 25485–25490 (2010).
56. Rosner, M. et al. mTOR phosphorylated at S2448 binds to raptor and rictor.
Amino Acids 38, 223–228 (2010).
57. Foster, K. G. & Fingar, D. C. Mammalian target of rapamycin (mTOR): conducting the cellular signaling symphony. J. Biol. Chem. 285, 14071–14077 (2010).
58. Soliman, G. A., Acosta-Jaquez, H. A. & Dunlop, E. A. mTOR Ser-2481 autophosphorylation monitors mTORC-specific catalytic activity and clarifies rapamycin mechanism of action. J. Biol. Chem. 285, 7866–7879 (2010).
59. Caron, E. et al. A comprehensive map of the mTOR signaling network. Mol.
Syst. Biol. 6, 435 (2010).
60. Sun, X., Threadgill, D. & Jobin, C. Campylobacter jejuni induces colitis through activation of mammalian target of rapamycin signaling. Gastroenterol
142, 86–95.e85 (2012).
61. Krisanaprakornkit, S., Kimball, J. R. & Dale, V. A. Regulation of human betadefensin-2 in gingival epithelial cells: the involvement of mitogen-activated protein kinase pathways, but not the NF-kappaB transcription factor family. J.
Immunol. 168, 316–324 (2002).
62. Moon, S. K. et al. Activation of a Src-dependent Raf-MEK1/2-ERK signaling pathway is required for IL-1alpha-induced upregulation of beta-defensin 2 in human middle ear epithelial cells. Biochem. Biophys. Acta 1590, 41–51 (2002).
63. Villageliú, D. N., Rasmussen, S., & Lyte, M. A microbial endocrinology-based simulated small intestinal medium for the evaluation of neurochemical production by gut microbiota. FEMS Microbiol. Ecol. 94, fiy096 (2018).
64. Qiu, Z. & Sheridan, B. S. Isolating lymphocytes from the mouse small intestinal immune system. J. Vis. Exp. 132, 57281 (2018).
65. Trapecar, M. et al. An optimized and validated method for isolation and characterization of lymphocytes from HIV+ human gut biopsies. AIDS Res.
Hum. Retroviruses 33, S31–S39 (2017).
66. Achanta, M. et al. Tissue expression and developmental regulation of chicken cathelicidin antimicrobial peptides. J. Anim. Sci. Biotechnol. 3, 15 (2012).
67. Szklarczyk, D. et al. STRING v10: protein−protein interaction networks, integrated over the tree of life. Nucleic Acids Res. 43, D447–D452 (2015).













.jpg&w=3840&q=75)